方案详情文
智能文字提取功能测试中
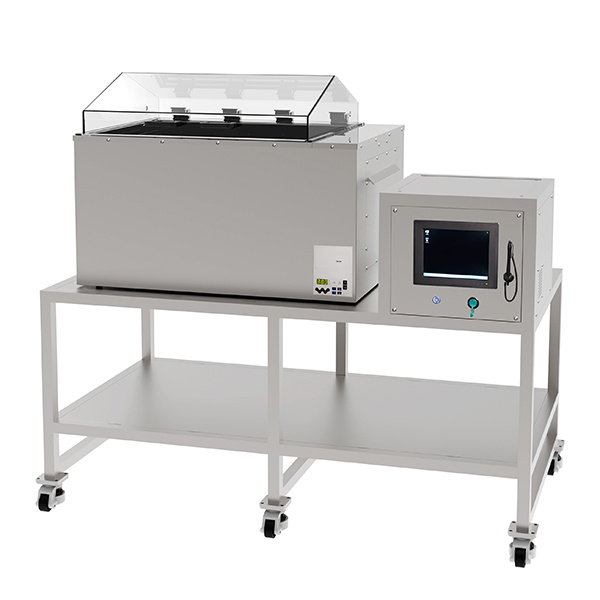
ThawSTAR@Automated Cell Thawing System Standardized thawing using breakthrough solid-state technology Introduction Advances in cryopreservation techniques over the lastfifty years12 have helped enable progress in a widerange of fields including cell biology research, drugdiscovery,biobanking, assisted reproduction, plant andanimal conservation, cellular therapy, and regenerativemedicine. While cryopreservation techniques haveimproved markedly, downstream thawing techniqueshave been largely overlooked, even though manyreports show that non-standardized thawing methodscan have deleterious effects on cryopreservedproducts35. The success of high promise fields suchas cellular therapy and regenerative medicine willrequire reproducible and standardized handling ofthe therapeutic cells6.7, including thawing duringmanufacturing and prior to patient administration toensure effective patient responses. This white paper describes in detail Astero Bio'sThawSTAR Automated Cell Thawing System (Figure 1),a first-of-its-kind automated thawing instrument thatis designed to de-risk thawing of live cell therapeutics.ThawSTARrapidly thaws the live biological contentsof a cryogenic vial with high reproducibility andminimal risk of contamination, thereby bringingstandardization to this critical step in the process.Topics covered in this white paper include features andutilization of the instrument, as well as performancedata. Standardizing Cell Thawing is Critical Cryopreservation has become an invaluable techniquewithin the biological sciences where cells and tissuesare routinely handled. Stem cells, genetically modifiedimmune cells, tumor cells and cell lines, bone marrowand cord blood-derived cells are examples of cell typesregularly cryopreserved by clinicians. Optimal thawing of these cells is critical to successful downstreamresearch. A broad range of applications such ascell therapy, cell-based drug discovery, biobankingreproduction and other cell-based assays can benefitfrom standardized cell thawing to increase theirproductivity and assist in fulfilling their missions toimprove human health. As these industries continue to expand their collectionsof cryopreserved samples, the need for minimizingvariability in sample handling through automationand standardization becomes essential8-10. Improvingcryopreservation techniques, including thawing, tomaximize viability and function of cryosensitive cellssuch as stem cells, hepatocytes" or neurons12 is vital toregenerative transplant medicine. The success of thecell therapy industry is likewise dependent on havinghigh quality, consistent products. Cryopreserved cells,whether they are being used as a primary treatment,or a reagent for cell-based discovery assays, drivethe need for optimized cell thawing and resuscitationmethods13. For controlled animal breeding, optimization Figure 2: ThawSTARCFT Transporter The ThawSTARCFT Transporter is engineered to hold cryogenic vials atnear dry ice temperatures prior to thawing them in ThawSTAR System.Dry ice is placed in the foam holder below the metal CFT2 Core. To verifythe holding temperature, a cryotube filled with cryopreservative solutionwith a centrally-located thermocouple was frozen in LN2 then transferredto the pre-equilibrated Transporter. The temperature profile shows thatthe vial warms quickly (<10 min) to the holding temperature and remainsstable for >1 hr. of freezing and thawing protocols for semen14hasenabled more efficient insemination as a result ofreduced spermatozoa damage. As part of a strategic vision to develop products thatimprove standardization of the entire cryopreservationworkflow, Astero Bio has identified cell thawing as oneof the most critical points in the process. As describedbelow, the ThawSTAR@ Automated Cell Thawing Systemwas engineered to provide an intuitive and reproduciblesolution for thawing cryogenic vials in research,manufacturing and clinical settings. Current Thawing Methods Biophysics and Biology of Cell Thawing.Cryopreservation of cells and tissues has been studiedextensively for decades. In its most basic form,effective cryopreservation (not accomplished bydirect vitrification) requires controlled-rate cooling ofthe cells generally in the presence of cryoprotectantto allow (a) minimization ofintracellular ice crystalformation during the liquid-to-solid phase transitionby effective cell dehydration, (b) control of osmoticgradients across the cell membrane as extracellularsolute concentrations increase, and (c) minimization ofextracellular ice crystal size. The microscopic processesoccurring upon the thawing of cryopreserved cells andtissues are almost mirror images of those that occurduring freezing: warming of the sample from cryogenictemperatures toward the solid-to-liquid phasetransition, melting of extracellular ice crystals to formliquid water, rehydration of the cells, and reformation ofan extracellular salt and protein solution. During a thaw, it is critical to minimize bothosmotic shock to the rehydrating cells and overallice recrystallization in the thawing mixture1.4,5,15-17.Ice recrystallization during thawing is a commonlyobserved phenomenon where small ice crystalsgenerated during the freezing process can reforminto larger crystals at sub-freezing temperatures andact as nucleation sites for the liquid water formed athigher temperatures5,15,16, The result of either processis progressively larger ice crystal formation that canbe injurious to cells. Temperature fluctuations or slowwarming of a frozen sample will increase ice crystalsize. The extent of damage from ice recrystallizationduring cell thawing can range from very minor tosignificant depending on the thaw procedure16-19.Decades of empirical results have demonstrated thatrapid, controlled thawing of cryopreserved samplesprovides optimal post-thaw viability for the majorityof cells and tissues by limiting ice recrystallizationand rehydrating cells as rapidly as possible. Ideally,thawing rate and temperature should also be optimizedfor cell size and volume, cell type, and choiceof cryopreservative. Current Methods for Cell Thawing. To achieve rapid thawing rates, biologists routinely plunge frozensamples into water of varying temperatures (from 37°Cup to 60°C) for seconds to minutes. By far, the mostcommon and well-accepted method for rapidly thawingcryopreserved cell samples is partial submersion of thevial in a 37°C water bath. There are several reasons forusing this approach: water baths are relatively cheapand easily available, they allow efficient heat transferfrom the water to the vial due to the high heat capacityand thermal conductivity of liquid water, and thereis little danger of“over cooking”the cells since themaximum temperature the vial can achieve is 37°C. However, there are significant disadvantages to usinga water bath for thawing, particularly in a clinicalenvironment. These disadvantages include: (1) lackof scalability post-manufacturing,(2) user-to-uservariability in subjectively determining thaw times,final vial temperature, and end point, (3) no datamanagement or chain-of-custody connectivity, (4)high risk of contamination of vial contents throughwicking of water into the cap threads and seal in apoorly maintained, and often communal, water bath,(5) inability to use a water bath as part of a sterileprocess inside a cell culture hood, (6) restrictions inusing a water bath in a GMP or clinical environment.To overcome some of the limitations of using a waterbath for thawing,researchers and process engineershave explored other options such as dry bead bathsor heat blocks20,21. Unfortunately, these solutions havevery inefficient thermal contact, resulting in reducedheat influx, and can take 2-3 times longer (~7 minutes ina dry bead bath vs.~2.5 minutes in a 37°C water bath)to thaw samples, which can increase the risk of icerecrystallization damage. Figure 3: Thermal Profile of Vials Thawed in a WaterBath or ThawSTAR System 1.8mL cryogenic vials filled with 1 mL of cryopreservation medium (10%DMSO/20% FBS/70% DMEM) were fitted with an interior wall thermocouple(< 0.5 mm from internal wall surface) and a central axis thermocouple,frozen at -80°C, and maintained at -75°C in a CFT2 Core on dry ice as inFigure 2. Three vials were thawed in a37°C water bath (left panel) or in theThawSTAR@System (right panel). The temperature profiles recorded byboth thermocouples were very similar for both the water bath thaw and theThawSTAR thaw. For the water bath thaw, the vials were removed from thebath when a pea-sized ice chunk remained (arrow) and then gently tappedto melt the chunk. Similarly, ThawSTAR ejected the vial at the point wherea pea-sized ice chunk remained (arrow) and after mixing the final vial tem-perature is ~5-10°C. Note that the sharp rise in temperature seen with thecentral thermocouple is indicative of the ice chunk breaking away from thethermocouple. As demonstrated below, the ThawSTARAutomatedCell Thawing System is designed to optimize and de-risk cell thawing at point-of-care. ThawSTAR@ providesan innovative solution for standardized, reliable, andhighly reproducible cell thawing that is equivalent orsuperior in performance to an ideal water bath-basedthaw and can be integrated into processes withinresearch, GMP, and clinical settings. ThawSTAR Thawing Platform ThawSTARAutomated Cell Thawing System (Figure1) is a compact instrument that uses solid-stateheating blocks with a pliant conductive materialinterface to maximize contact and heat transfer to vialsbeing thawed. The patent-pending STAR'M sensingtechnology monitors vial temperature and utilizessoftware algorithms to detect the solid-to-liquid phasechange. Astero Bio recognizes that cell type, cell sizeand volume, and choice of cryopreservative all affectoptimal thawing rate and temperature. Each ThawSTARsystem can be programmed with a customized thawingalgorithm, specific to a given cell therapy product orcell type, in order to preserve optimal function. Theresult is a reproducible and standardized thaw for vialstaken directly from LN, storage,a -80°C freezer, orthose equilibrated and held at to dry ice temperature(-78.5°C) in the ThawSTAR CFT Transporter (Figure2). The ThawSTAR Automated Cell Thawing Systemis designed to thaw cryogenic vials similarly to a waterbath in terms of heat influx rate and final temperatureachieved, resulting in cell viability and recovery rates Figure 4: Thawing Vials Directly from LN, Storage 1.8 mL cryogenic vials filled with 1 mL of cryopreservation medium (10%DMSO/20% FBS/70% DMEM) were fitted with an interior wall thermocouple(<0.5 mm from internal wall surface) and a central axis thermocouple andfrozen at -196°C. The vials were removed from LN2 and immediate placedin the ThawSTAR instrument. The ThawSTAR"ejected the vial at the pointwhere a pea-sized ice chunk remained (arrow). Note that the sharp rise intemperature seen with the axial thermocouple is indicative of the ice chunkbreaking away from the thermocouple. Final vial temperature is~5-10°C,comparable to a water bath thaw. that are statistically identical to or superior to thoseachieved with a water bath. Furthermore, ThawSTAR@Automated Cell Thawing System eliminates the riskof water borne contamination, and the variability inthawing times and endpoints associated with using awater bath. Breakthrough Technology for Solid-State Thawing.The ThawSTAR@solidstate technology platform isengineered to provide a heating profile and final vialtemperature similar to that achieved when thawingin a 37°C water bath. This is achieved by usingconductive heating blocks that are coupled to the vial Figure 5: Thaw Time Reproducibility of the ThawSTAR Left panel: The average time for the same ThawSTAR System to thaw> 5 frozen vials each day for 5 days.Right panel: The average thaw timefor three different ThawSTARSystems was measured using> 5 frozenvials per unit on one day. No significant differences were identified foreither scenario at p<0.05 (2-way ANOVA with post hoc Sidak test). Forcomparison, six vials were thawed in a 37°C water bath. The average thawtime in the water bath was 151 seconds, with a 99% confidence interval of139-164s (range shown as dotted lines). Figure 6: Rapid Vial Thawing with ThawSTARCompared to Dry Bead Bath or Heat Block 1.8 mL cryogenic vials filled with 1 mL of cryopreservation medium (10%DMSO/20% FBS/70% DMEM) were fitted with a wall thermocouple (<1 mmfrom internal wall surface) and a central axis thermocouple, frozen at -80°C,and maintained at -75°C in a CFT2 Core on dry ice as in Figure 2. Vials werethawed in either a ThawSTAR° System (green traces), a 37°C bead bath(Lab Armor beads; red traces), or an aluminum heat block equilibrated to37°C (blue traces). The ThawSTARSystem thaw time is 2-3X faster thanthese other dry thawing methods. to be thawed through an inert, malleable, conductivematerial that conforms to any irregularities in the vialwall, thus providing a uniform heat transfer surface.This coupling solves the problem of inefficient heattransfer commonly seen with other solid state thawingprocesses such as dry bead baths or bare metalheating blocks. The thermal profile of vials thawed in aThawSTAR System is virtually identical to that seen ina water bath (Figure 3) including heating rate and finalvial temperature. The ThawSTARtechnology monitors the vialtemperature during initial heating and detects the pointat which the contents initiate phase change from solidto liquid. Labels or writing on the cryogenic vial do notaffect the performance of the unit. This unique feature Figure 7: Thawing of Peripheral Blood MononuclearCells Cell viability (left panel) and recovery (right panel) of PBMC were measuredusing trypan blue exclusion on a hemacytometer. Recovery is the numberof viable cells post-thaw as a percentage of the pre-freeze viable cells. Nostatistical difference in viability (2-way ANOVA with post hoc Sidak test) orrecovery (unpaired two-tailed t-test) at p<0.05 were found. Data courtesyof Dr. Mars Stone at the Blood Systems Research Institute. of the ThawSTAR System ensures active detection ofthe phase change initiation, enabling successful vialthawing from LN, temperatures (Figure 4) in additionto dry ice temperatures. In addition, the ThawSTAR@System can thaw samples stored at -20°C,enabling controlled thawing of antibody, enzyme, orother biospecimen aliquots. The performance of the ThawSTAR@ System'shardware and software algorithms are highly reliable,enabling the System to be a powerful standardizationtool. Figure 5 demonstrates the high run-to-runreproducibility of a single unit when multiple vials werethawed on different days. Additionally, high unit-to-unit reproducibility was alsodemonstrated by testing multiple units on the sameday. The average thawing time of 1.0 mL of frozencell suspension with a ThawSTAR System was 160 s;statistically equivalent to the average thaw time of 151s obtained when using a water bath. The ThawSTARSystem thaws a vial 2-3X faster than other commonlyused dry thawing methods (Figure 6), thus minimizingthe risk of ice recrystallization damage to the cells. Instrument Validation by Effective Thawing of MultipleCell Types. The ability of the ThawSTAR System toeffectively thaw cryopreserved cells was analyzedby multiple independent investigators in a head-to-head comparison with the standard 37°C water baththawing method (Figures 7 and 8). In each case, 6vials of the same lot of frozen cells were removed fromLN,stores, randomly assigned to either a“37°C waterbath”or“ThawSTAR@”group,equilibrated to dry icetemperatures in a CFT2 Core placed in dry ice, thenthawed by either method. In each case, cell count andviability (or recovery of viable cells) were assessedimmediately post thaw (day 1) and after 3 days ofgrowth or recovery (day 3) as described in the figurelegends, and the results compared statistically. Figure 8: Thawing of K562 Erythromyeloblastoid Cells Cell count (left panel) and viability (right panel) of K562 cells weremeasured using trypan blue exclusion on a hemacytometer. No statisticaldifference in viability or cell count (each tested with 2-way ANOVA withpost hoc Sidak test) at p<0.05 were found.Data courtesy of Helen Huls atthe MD Anderson Cancer Center. Figure 9: Higher Post-Rest Average Recovery Average recovery post-rest (16-24 hrs). The post-rest recovery is the ratioof the total number of viable cells postrest and the total number of viablecells post-thaw multiplied by 100%. For each donor, the data is expressedas the average of the post-rest recovery triplicates. The percentageswritten on the figures represent the mean of the average recovery for alldonors. The results are based on 6 independent runs (n = 17 vials for waterbath and n = 17 vials for ThawSTAR@instrument).* ps0.05(p=0.0333).Data courtesy of Caprion BioSciences and McGill University. The ThawSTAR@ System showed statistically equivalentresults compared to a water bath for all cell typestested including peripheral blood mononuclear cells(PBMC;Figure 7), the K562 erythromyeloblastoidcell line (Figure 8),as well as human splenocytes,stimulated CD8+ central memory T cells, and antibodyproducing mouse hybridoma cells (data not shown).Studies also showed significantly higher post-restrecovery in PBMCs thawed with the ThawSTAR@system as compared to those thawed by water bath(Figure 9). This data is significant because it has beendemonstrated that apoptosis and necrosis arisingfrom the stress of the thawing procedure reaches itspeak 24 hours post-thaw2. It is therefore likely thatthe ThawSTARSystem subjects PBMCs to less stressduring the thawing procedure than water bath thawing.Taken together, these results demonstrate that theThawSTARAutomated Cell Thawing System canachieve identical or superior cell recovery and viabilitycompared to the standard 37°C water bath thawingmethod. Summary ThawSTAR Automated Cell Thawing System is anintuitive, fully automated system designed to de-riskand standardize clinical cell thawing. It is engineeredto reproducibly thaw the live biological contents ofa cryogenic vial in a similar manner to the commonlyused 37°C water bath but without the subjectivity orrisk of contamination found with water bath usage.The intuitive operation of the ThawSTAR System can be readily integrated into most current workflows withthe added advantage of easy adoption into sterileprocedures performed inside a cell culture hood, GMPor clinical setting. The ThawSTAR Automated CellThawing System standardizes the“last mile” in thecryopreservation workflow and enables future cell-based discoveries and therapies. About Astero Bio Astero Bio develops and commercializesstandardization and automation technologies for vitalpreclinical and clinical sample handling. An industryfirst, the ThawSTAR Automated Cell Thawing Systemreplaces uncontrolled and highly variable manualmethods with a customizable algorithm for each uniquecell therapy product. Astero Bio's global customersinclude pharmaceutical, medical, stem cell and otherGMP facilities where consistent and repeatableoutcomes are paramount. References 1.Mazur, P., et al. (1970)Interactions of cooling rate, warmingrate, and protective additive on the survival of frozenmammalian cells. Ciba Foundation Symposium on the FrozenCell. J&A Churchill Publication,London,UK. 2. Bissoyi, A., et al. (2014) Targeting cryopreservation-inducedcell death: a review. Biopreserv Biobank. 12(1):23-34. 3.http://www.bioprocessintl.com/wp-content/uploads/bpicontent/BPI_A_110904AR11_O_145195a.pdf 4.Fowler, A. and Toner, M. (2005) Cryo-injury andbiopreservation. Ann N Y Acad Sci. 1066:119-135. 5. Chaytor, J.L.,et al.(2012) Inhibiting ice recrystallizationand optimization of cell viability after cryopreservation.Glycobiology.22(1):123-133. 6.Yang, H., et al. (2014) Effects of interruptions of controlled-ratefreezing on the viability of umbilical cord blood stem cells.Transfusion. doi: 10.1111/trf.12774. 7.Li, Y., and Ma, T. (2012) Bioprocessing of cryopreservationfor large-scale banking of human pluripotent stem cells.BioResearch Open Access. 1(5):205-214. 8.Peakman, T.,et al.(2010) Current standards for the storage ofhuman samples in biobanks. Genome Medicine. 2:72. 9. Querol, S., et al. (2010) Quality rather than quantity: the cordblood bank dilemma. Bone Marrow Transplantation. 45:970-978. 10. Cuhadar, S., et al. (2013) The effect of storage time andfreezethaw cycles on the stability of serum samples. BiochemiaMedica. 23(1):70-7. 11. Terry, C., et al. (2010) Optimization of the cryopreservationand thawing protocol for human hepatocytes for use in celltransplantation.Liver Transplantation. 16:229-237. 12. Shi, Y. et al. (2012) Directed differentiation of humanpluripotent stem cells to cerebral cortex neurons and neuralnetworks. Nature Protocols. 7(10):1836-46. 13. Guido, J.R., et al.(2007) Cryopreserved cells facilitate cell-based drug discovery. Drug Discovery Today.12:13-14. 14. Bradford, L.L. and Buhr, M.M. (2002) Function of cryopreservedhorse semen is improved by optimized thawing rates. J EquineVet Sci. 22(12):546-550. 15. Cao, E. et al. (2003) Effect of freezing and thawing rates ondenaturation of proteins in aqueous solutions. BiotechnolBioeng.82(6):684-90. 16. Carpenter, J.F. and Hansen, T.N. (1992) Antifreeze proteinmodulates cell survival during cryopreservation: Mediationthrough influence on ice crystal growth. Proc Natl Acad SciUSA. 89:8953-8957. 17. Deller, R.C., et al.(2014) Synthetic polymers enable non-vitreous cellular cryopreservation by reducing ice crystalgrowth during thawing. Nature Communications. 5:3244. 18. Norkus, M. et al.(2013) The effect of temperature elevation oncryopreserved mesenchymal stem cells. Cryoletters. 34(4):349-359. ( 1 9 . Olson, W .C., e t al. (2011) Shipping blo o d to a central la b oratoryin multicenter clinical tr i al s : Effect of ambient te m peratureon specimen temperature, and e f fects of temperature onmononuclear cell yield, v iability and immunologic function. J T rans M ed. 9(26):1- 1 1. ) ( 20.Rollig, C . , et al. (2002) Thawing of cryopreserved mobilizedper i p h eral blood--comparison between waterbath and drywarming device. Cytotherapy. 4(6): 5 51-5. ) ( 21 . Triana, E., e t al. (20 1 3) Thawing of cryopreservedhematopoietic progenitor cells from apheresis with a n ew dry-warm i ng device. T r ansfusion. 5 3 (1):85-90. ) ( We would like to thank the following contributors: Dr. M ars Stone,Blood Systems Research Institute, Helen Huls, MD AndersonCancer Center and Caprion BioSciences a n d McGill Un i versity. ) @2018. Astero Bio Corporation. All rights reserved. Patents pending. 美国百奥莱BioLife Solutions公司推出的ThawSTAR 无水干式细胞复苏仪,为-196℃液氮下存储、-80℃超低温冰箱等极端低温的生物样品解冻复苏工艺提供了更安全更方便的方法。下面我们介绍下的ThawSTAR CFT2 是一款针对冻存管生物样品的解冻复苏利器: 传统的细胞解冻方式:37℃水浴锅或者手捂揉搓方式 新方法:ThawSTAR®细胞程序复苏* 取决于操作者实战经验判断复苏终点 * 无需手动操作解冻* 多样化的复苏终点 * 高度重复标定终点* 潜在污染风险 * 避免污染风险* 无法工艺标准化 * 标准化的工艺方法ThawSTAR®自动解冻复苏系统采用专利温控传感技术STARTM准确的判断识别解冻复苏终点,适用于存储在-80℃低温冰箱或者气相液氮条件下的生物样本。结合配套低温转运盒(干冰)可以有效保持复苏后的细胞活率。操作简单,仅需三步!对比实验:6个冻存管在37℃水浴池里,平均解冻时间终点时间在151秒(计时确认139秒~164秒范围)左边的数据:每天重复实验,连续检测5天。右边数据,多于5支冻存管,每天在3台ThawSTAR CFT2细胞复苏仪内进行复苏实验,实验数据与水浴效果基本相当,无明显区别。B 细胞连续解冻复苏细胞活率,传统水浴与ThawSTAR对比PBMC人体外周血单核细胞复苏后活率,传统水浴与ThawSTAR对比PBMC人体外周血单核细胞连续复苏后活率,传统水浴与ThawSTAR对比间充质干细胞复苏后活率,传统水浴与ThawSTAR对比(以上信息由授权代理上海朗喜工业科技有限公司提供,未经允许禁止转载!)
关闭-
1/6

-
2/6

还剩4页未读,是否继续阅读?
继续免费阅读全文产品配置单
上海朗喜工业科技有限公司为您提供《冻存细胞中复苏后的细胞活率检测方案(细胞复苏仪)》,该方案主要用于其他中复苏后的细胞活率检测,参考标准《暂无》,《冻存细胞中复苏后的细胞活率检测方案(细胞复苏仪)》用到的仪器有ThawSTAR 细胞程序复苏仪(冻存管)、ThawSTAR细胞程序复苏仪、法国卡苏CBS细胞程序降温仪、CryoHandy便携气相液氮转运杯、美国百思臻 细胞降温 梯度降温盒。
我要纠错
推荐专场
相关方案










 咨询
咨询


