方案详情文
智能文字提取功能测试中
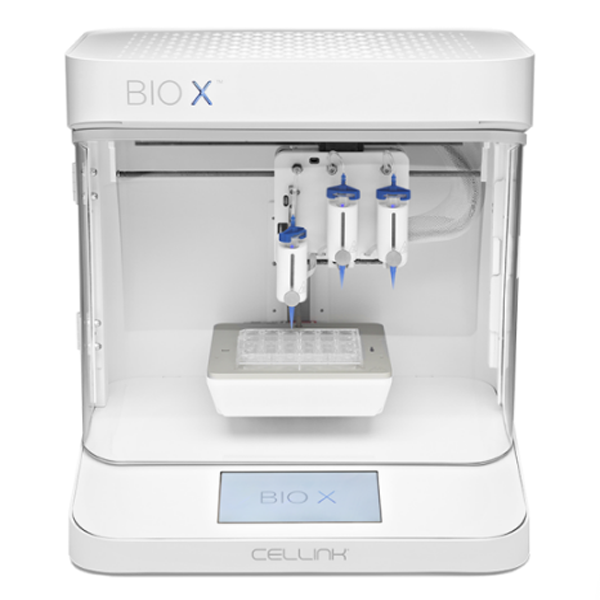
3D 打印技术允许通过高精度逐层沉积材料,以定制的几何形状和成分自动和可重复地制造用于组织工程的功能结构。 出于这些目的,生产由生物相容性材料制成的生物活性凝胶基 3D 支架具有明确的内部结构,包括双重(中孔和大孔)和高度互连的孔隙率。 在这项工作中,用于骨再生目的的气凝胶支架是通过一种创新策略获得的,该策略结合了海藻酸盐-羟基磷灰石 (HA) 水凝胶的 3D 打印和凝胶的超临界 CO2 干燥。 进行 BET 和 SEM 分析以评估获得的气凝胶支架的结构参数,并评估原始计算机辅助设计 (CAD) 设计的尺寸精度。 还对气凝胶支架进行了关于细胞活力、粘附和迁移能力的生物学表征。 获得的藻酸盐-HA 气凝胶支架具有高度多孔性、生物相容性、对 CAD 模式的高保真度,还允许间充质干细胞 (MSC) 的附着和增殖。 在测试的气凝胶制剂存在的情况下,观察到成纤维细胞向受损区域迁移的增强,这在骨再生方面是积极的。Materials Science& Engineering C 131(2021) 112525A. Iglesias-Mejuto and C.A. García-Gonzaalez Contents lists available at ScienceDirect Materials Science& Engineering C journal homepage: www.elsevier.com/locate/msec 3D-printed alginate-hydroxyapatite aerogel scaffolds for bone tissue engineering Ana Iglesias-Mejuto, Carlos A. García-Gonzlalez* Department of Pharmacology, Pharmacy and Pharmaceutical Technology, I+D Farma group(GI-1645), Faculty of Pharmacy and Health Research Institute of Santiago de Compostela(IDIS), Universidade de Santiago de Compostela, E-15782 Santiago de Compostela, Spain Keywords:3D-printing Supercritical drying Aerogel Bone scaffold Hydroxyapatite A B S T R A C T 3D-printing technology allows the automated and reproducible manufacturing of functional structures for tissue engineering with customized geometries and compositions by depositing materials layer-by-layer with high precision. For these purposes, the production of bioactive gel-based 3D-scaffolds made of biocompatible mate-rials with well-defined internal structure comprising a dual(mesoporous and macroporous) and highly inter-connected porosity is essential. In this work, aerogel scaffolds for bone regeneration purposes were obtained by an innovative strategy that combines the 3D-printing of alginate-hydroxyapatite(HA) hydrogels and the su-percritical CO2 drying of the gels. BET and SEM analyses were performed to assess the textural parameters of the obtained aerogel scaffolds and the dimensional accuracy to the original computer-aided design(CAD) design was also evaluated. The biological characterization of the aerogel scaffolds was also carried out regarding cell viability, adhesion and migration capacity. The obtained alginate-HA aerogel scaffolds were highly porous, biocompatible, with high fidelity to the CAD-pattern and also allowed the attachment and proliferation of mesenchymal stem cells(MSCs). An enhancement of the fibroblast migration toward the damaged area was observed in the presence of the aerogel formulations tested, which is positive in terms of bone regeneration. 1. Introduction Bone defects resulting from tumors, infections, trauma, biochemical disorders and abnormal skeletal developments generate severe health problems and represent high sociosanitary costs for the national health services [1]. Biological grafts (autografts, allografts) and non-degradable grafts(metallic and ceramic implants) are the most com-mon solutions for these pathologies. However, their low availability(for biological grafts) and frequent post-surgical complications such as the lack of osseointegration or the generation of immune response(for non-degradable grafts) are among the important drawbacks that may occur [2]. Regenerative medicine aims to anatomically and functionally restore damaged tissues using a combination of(i) advanced biode-gradable 3D-scaffolds as temporary extracellular matrices(ECM),(ii) cells, and(iii) growth factors[2,3]. The processing method used to obtain these bone scaffolds should provide an optimum design to pro-mote the new tissue formation. These bone scaffolds should have a well-defnied internal structure, dual interconnected porosity and bioactivity. Given the increasing complexity in morphology and composition of these structures and the high sensitivity to processing environments(e. g., high temperature, shear stress, pH, use of organic solvents), inno-vative and benign strategies are sought to generate these new biomed-ical products[4]. 3D-printing is a cutting-edge technology that allows the automated and reproducible fabrication of functional, scalable and customized artifciial structures for personalized medicine [5]. In general, this technology uses a layer-by-layer deposition of biocompatible materials to achieve stable 3D-constructs. Specifcially, extrusion-based bio-printing is an additive manufacturing technique commonly used to create hydrogel scaffolds[6,7]. It is a pressure-based method that em- ppllooyyss aa rroobboottiicc ssyysstteemm lliinnkkeedd ttoo aa bbiiooiinnkk ddiissppeennssiinngg ssyyrriinnggee.. AA computer-aided design(CAD) is used to deposit the bioink in a 3D-pre-defnied shaped structure. This technique is able to print different tissues with the generation of anatomically correct macroporous structures[8]. A limited(but growing) number of biomaterials are suitable for bioink formulations to generate 3D-printed scaffolds as they must be printable, biocompatible and present attractive structural and mechanical prop-erties[9]. Nevertheless, structures obtained by 3D-printing have the customized external morphology essential for personalized medicine, but tthheeyy uussuuaallllyy llaacckk tthhee hhiigghh pprreecciissiioonn rreeqquuiirreedd ttoo ggenerate https://doi.org/10.1016/j.msec.2021.112525 Received 30 July 2021; Received in revised form 18 October 2021; Accepted 23 October 2021 Available online 27 October 2021 0928-4931/© 2021 The Authors. Published by Elsevier B.V. This is an open access article under the CCBY license(http://creativecommons.org/licenses/by/4.0/). nanostructured scaffolds, with a control in the macro and microstruc-tural levels. For this reason, the combination of 3D-printing with other techniques is needed to yield customized nanostructured biomaterials. Polymeric nanostructures with advanced properties can be obtained using supercritical fulid technology based on the use of supercritical carbon dioxide(scCO2)[10]. Namely, scCO2-assisted drying is adequate for the extraction of the solvent of a gel while preserving the internal gel structural properties, such as high porosity and high specifci surface areas, in the so-called aerogels. This technology can be used to obtain aerogel-containing grafts and implants[11], among them aerogel bone scaffolds for tissue engineering applications[12–14]. Aerogels present a high mesoporosity comparable to that of the native ECM, which favor cell growth, and can be obtained from polysaccharides and proteins [15]. Alginate is a natural biopolymer widely used for bone scaffolds and for bioink formulation because it is biocompatible, biodegradable, non-toxic and non-immunogenic, and supports cell growth[16]. Alginate generates a stable hydrogel in the presence of low concentrations of divalent cations, namely Ca2+ which presents the advantage of its low toxicity with respect to other divalent ions. Finally, alginate composition resembles glycosaminoglycan(GAG) structure, one of the major com-ponents of the natural ECM in human tissue. However, alginate-based structures usually lack bioactivity and should be combined with other admixtures for bone tissue engineering purposes[17]. Hydroxyapatite(HA) is the major inorganic component in mamma-lian hard tissues and also an excellent bone substitute material because it is bioactive, osteoconductive, non-toxic and highly biocompatible due to its chemical and structural similarity to natural bone minerals[18,19]. This chemical similarity is essential for apatite deposition and subse-quent bone regeneration. HA may also have a role as a cross-linking agent and as an inorganic mechanical reinforcer[20]. Moreover, HA and its composites are suitable for attachment, proliferation and dif-ferentiation of mesenchymal stem cells(MSCs). All these properties render HA favorable for osteointegration[21–23]. The source and size of HA particles is an important factor on alginate-HA gel scaffolds, because the HA grain size and specifci surface area affect the gelling time and rheological properties of the hydrogels. MicroHA has been proposed for applications requiring rapid gelation kinetics and improved mechanical properties, while nanoHA is appropriate to render homogeneous hhyyddrrooggeellss uunnddeerr mmoorree ccoonnttrroolllleedd ggeellaattiioonn kkiinneettiiccss [[2200]].. OOvveerraallll,, alginate-HA composites are promising candidates for bone tissue engi-neering where HA also triggers the mineralization process and stimu-lates calcium phosphate and HA nanocrystals nucleation and growth [19,21]. Strategies for the generation of a complex 3D-shaped structures with different functionalities and architectures ranging from the nanoscale to the macroscale are under development to generate structures with this pore hierarchy[24]. The design and optimization of the fnial pore structure(pore size hierarchy and proportions) is also essential for the material performance in tissue engineering applications. The use of aerogel technology can solve some of the current 3D-printing limitations regarding the nanostructuration of 3D-scaffolds, but the production of aaeerrooggeellss wwiitthh aa ccuussttoommiizzeedd eexxtteerrnnaall mmoorrpphhoollooggyy iiss aa rreemmaaiinniinngg remarkable challenge[25]. Recently, several 3D-printed aerogels have shown an excellent printability in the wet state and the preservation of their textural properties like a high specifci surface area[25–27]. Nevertheless, aerogels usually lack macroporosity and methods to confer it and to control the macropore size are under development [28,53–55]. In general, aerogels with various pore size ranges are highly desirable for applications like bone tissue engineering[29]. The unexplored combination of 3D-printing and aerogel technolo-gies for bone tissue engineering is herein proposed as a win-win strategy to obtain biomaterials with improved performance and architecture. Finally, new strategies to improve the aerogels strengthening and the printing process necessary to obtain more fnie and intricate structures are still a challenge nowadays. In this work, 3D-printed alginate aerogel scaffolds containing hydroxyapatite were processed by a combination of 3D-printing of hydrogels and supercritical CO2 drying for bone regen-eration purposes. The effects of alginate, HA and Ca2+concentrations on the 3D-printed hydrogel scaffolds processability were assessed. Then, the 3D-printed aerogels obtained after supercritical drying were evalu-ated regarding their textural(specifci surface area, porosity, density, shrinkage) and biological (cyto- and hemocompatibility, adhesion, migration) properties. The fdielity of the different gel formulations with respect to the original CAD flie was also evaluated. 2. Materials and methods 2.1. Materials Alginic acid sodium salt from brown algae with medium viscosity (guluronic acid/mannuronic acid ratio of 70/30, Mw 403 kDa, 3170cps) and calcium chloride(CaCl2; Mw 110.98 g/mol, 99.99% purity) were provided by Sigma Aldrich(Madrid, Spain). Hydroxyapatite(HA; Mw 502.31 g/mol, reagent grade purity, micropowder) was provided by Fluidinova(Moreira da Maia, Portugal). CO2 (purity>99.9%) was supplied by Nippon Gases(Madrid, Spain) and absolute ethanol(EtOH) by VWR(Radnor, PA, USA). Water was purifeid using reverse osmosis (resistivity>18 MQ·cm; Milli-Q, Millipore®, Madrid, Spain). 2.2. 3D-printing of hydrogel scaffolds Aqueous bioinks with three different alginate concentrations(6, 8and 10 wt% with respect to water) were prepared using milliQ water as a solvent. Furthermore, different HA concentrations(0, 8, 16 and 24 wt%with respect to water) were added to the 6 wt% alginate solutions. All alginate solutions were prepared under vigorous agitation(600 rpm) employing a homogenizer(VWR vos 60, Pennsylvania, USA) for at least 1 h at room temperature(RT). The thus obtained alginate solutions were degassed in a sonication bath(Branson 3510 Emerson, Ferguson, MO, USA) for 10 min to eliminate air bubbles. Hydrogels were obtained by printing the alginate inks with a Cellink BIOX Bioprinter(Boston, MA, USA) at RT using an extrusion printhead with a 3-mL syringe and a 410-um nozzle at the printing pressure of 50 kPa and a printing velocity of 12 mm/s. 3D-printed alginate hydrogels with dimensions of 20x20x1mm(for physicochemical tests, cf. Sections 2.4 and 2.5) and 10x10x1mm(for biological tests, cf. Sections 2.6 to 2.8) were obtained using a grid pattern and 3 layers. After the printing process, all scaffolds were put directly in contact with CaCl2 aqueous solutions(0.1, 0.5 and 1 M) for gelation(Fig. S1 of Supplementary Info). 2.3. Supercritical drying of 3D-printed gels Alginate hydrogels turn alcogels by immersion in absolute EtOH. Two solvent exchanges to ethanol were carried out with an exchange frequency of 24 h. The alcogels were wrapped in fliter paper and dried by supercritical drying to obtain the aerogels. Briefyl, gels were placed into a 100-mL stainless steel autoclave(Thar Process, Pittsburg, PA, USA) and immersed in 25 mL of absolute ethanol to prevent them from shrinkage before being in contact with compressed CO2. scCO2 was supplied using a dual piston pump and introduced from the top of a vessel heated at the constant temperature of 40 °C. Firstly, a continuous CO2 folw rate(5–7 g/min) at 120 bar took place for 4 h. Aerogels were then obtained after CO2 depressurization at a rate of 2 bar/min, collected from the autoclave and stored for characterization. The ob-tained scaffolds were denoted as Alg x%,HA y%,CaCl2 zM(x= 6, 8,10 wt%; y= 8, 16, 24 wt%; z= 0.1, 0.5, 1 M). 2.4. Physicochemical characterization of alginate aerogel scaffolds The skeletal density of the aerogels(Pskel) was determined using a helium pycnometer(Quantachrome, Boynton Beach, FL, USA) at 25 ℃C and 1.01 bar. Values were obtained from fvie replicates. The apparent density of the aerogel scaffolds formulations(papp) was determined following the Eq.(1): where the volume of the aerogels was obtained by measuring the three dimensions of the aerogel obtained with a digital caliper(Fowler™, Newton, MA, USA). The porosity of the structures(e) was obtained from Eq.(2) from the specifci volume considering the external dimensions of the material(Vt) and the specifci volume occupied by the voids in the full volume(Vvoid,t). The inner porosity of the aerogel fbiers(ef) was obtained from Eq.(3) from the specifci volume occupied by the fbiers(Vfbiers) and the specifci volume occupied by the voids(i.e. pores) in the fbiers(Vvoid,fbiers). The volumetric shrinkage(in percentage) of the aerogel scaffolds was calculated from the external dimensions of the material before and after supercritical drying following the Eq.(5): Low-temperature N2 adsorption/desorption analysis(ASAP 2000Micromeritics Inc.; Norcross, GA, USA) was performed to assess aerogel textural properties. Before measurements, samples were degassed under vacuum at 40 °C for 24 h. Specifci surface area(ABET) of aerogels was evaluated employing the BET(Brunauer–Emmett–Teller) method. Spe-cifci pore volume(Vp), pore size distributions and mean pore diameter(dp) were determined applying the BJH(Barrett–Joyner–Halenda) method. The morphology of the aerogels was evaluated by scanning electron microscopy(SEM, EVO LS15, Zeiss, Oberkochen, Germany). Aerogel samples were iridium-sputtered prior to imaging to minimize charging and to improve the image quality. 2.5. Dimensional accuracy tests Two indices(printing accuracy and shape fdielity factor –SFF–) were employed to assess the fdielity of the gel structures(for alcogels and aerogels) with respect to the original printing flie processed by 3D-print-ing in the frist step of the dual processing strategy herein proposed. The printing accuracy and SFF were calculated from Eqs.(6) and(7), respectively: where Ai is the alcogel or aerogel printed area respectively, and A is the CAD area(printing flie). 2.6. Cell viability tests The cytocompatibility of the different alginate-HA aerogel scaffolds was determined by assessing the viability of mouse embryo fbiroblasts (BALB/c3 T3) after 24 and 48 h of culture in the presence of the aerogel formulations using the WST-1 test and in triplicate. This test is based on the degradation of WST-1 into formazan and is directly correlated with the number of metabolically active cells. BALB cells(6500 cells/cm2) were seeded in 24-well plates in DMEM supplemented with 15% fetal bovine serum, penicillin 100 U/mL and streptomycin 100 g/mL. Cells were incubated at 37 °C in a humidifeid atmosphere enriched with 5% CO2. Scaffolds(1 × 1 1 0.1 cm) were UV-sterilized for 1 h and then placed in the wells with cells containing 1500 pL of DMEM supplement. Positive controls of cells with 1000 uL of medium and blanks of 1000 uL of medium(both in triplicate) were maintained at the same conditions. After 24 and 48 h of culture, scaffolds were removed, 250 uL of medium was left in the wells and 25 pL of WST 1 reagent was added. The plate was incubated for 2 h at the same conditions and then shaken thor-oughly for 1 min. Finally, 110 pL were transferred to a 96-well plate to measure the absorbance at l=450 nm in a microplate reader(Infniite®M200, Tecan Group Ltd., Mannnedorf, Switzerland). 2.7. Cell attachment tests The spreading of human bone marrow mesenchymal stem cells (MSCs) onto the scaffolds was evaluated by DAPI staining to visualize the cellular nuclei after 6 and 13 days of culture[30]. MSC-seeded scaffolds were fxied with paraformaldehyde(4% wt/v) for 10 min and washed with PBS. Then, they were incubated in Triton/PBS(0.2% v/v) solution for 5 min. Finally, scaffolds were washed with PBS, placed on glass slides, and one drop of the DAPI-containing ProLong gold antifade mountant(Molecular Probes Inc., Eugene, OR, USA) was added to each scaffold before their storage at - 20 CC. Finally, cell attachment in the scaffolds was evaluated using a Leica TCS-SP2 spectral confocal micro-scope(Leica TCS-SP2, Leica Microsystems Heidelberg GmbH, Man-nheim, Germany)[31]. An open source software(ImageJ 1.5i, US National Institutes of Health, Bethesda, MD, USA) was used to analyze the captured images. 2.8. Migration assay Cell migration was evaluated by a scratch wound healing assay [32,33]. After the confulence, BALB cells monolayer was scratched by a straight line using a sterile pipette tip and mimicking a wound in vitro. PBS was then employed to wash cells and remove cell debris. The different aerogel scaffold formulations were placed in the wells with fresh cell culture medium at 37 °C. Photographs of the scratch wound were obtained with an inverted microscope(Olympus, Japan) immedi-ately(t= 0 h) and at 24 h to analyze the cell migration. The migration area(%) was assessed as follows(Eq.(8)): where A0 represents the initial wound area(t= 0 h) and An represents the residual wound area at 24 h measured by ImageJ software. 2.9. Statistical analysis Results of cell viability tests for each aerogel scaffold type(n= 3) were reported as mean value ± standard deviation. t-tests were carried out to determine the statistical signifciance of the differences among the groups, and values of p 0.05 were considered as statistically signifciant. 3. Results and discussion 3.1. Effect of alginate and CaCl2 concentration on scaffolds The feasible operating region of alginate ink formulation composi-tion and Ca2+ concentration ranges for 3D-printing was fristly deter-mined. The following criteria were followed:(i) alginate bioink must be liquid-like in the printhead to avoid the tip clogging, but(ii) it must be solid-like in the printbed to maintain the customized 3D-geometry during the deposition process and avoid the structural integrity loss. Homogeneous 3D-structures formed by differentiated fliaments ar-ranged in layers were accordingly obtained with alginate concentrations in the 6–10 wt% range and a CaCl2 concentration of 0.5 M(Fig. 1). Inks Fig. 1. SEM pictures of 3D-printed alginate aerogels prepared at CaCl2 concentration of 0.5 M and from aqueous alginate inks of different concentrations: a) 6, b) 8, and c) 10 wt%. Aerogels are observed at two different magnifciations. below or above this alginate concentration range were discarded due to the non-homogeneous appearance obtained for the 3D-printed hydro-gels. The 3D-structure and porosity, with mesopores and macropores, was clearly recognized in all aerogels produced in the feasible region. Tighter fbier interactions appear to be present at alginate concentrations of 10 wt%. A highly interconnected structure with mesopores and macropores was observed. An improvement in the textural parameters (ABET and Vp) in all aerogels was also observed(Table 1) with respect to other alginate aerogels previously described[34]. Ionic crosslinking of alginate gels provided long-term stability to fnial structures in the 0.1–1 M CaCl2 range. Alginate scaffolds cross-linked at this CaCl2 concentration range had a highly porous structure throughout the scaffold with a high aerogel surface area(Fig. 2 and Table 1). Finally, alginate scaffolds crosslinked with CaCl2 1 M solution had more homogeneously printed strands, which could be attributed to more Cat2 ions being involved in the ionic crosslinking of the alginate [35]. In general, aerogel scaffolds obtained at alginate concentration 6 wt% and gelifeid with CaCl2 1 M exhibited non-woven fbiers with tighter junctions if compared to the rest of formulations studied and resulting in less brittle constructs. High values of textural properties were obtained for all the tested aerogel formulations, although the composition and crosslinker con-centration had an infulence in the results(Table 1), being the highest values found in aerogels obtained from inks using an alginate concen-tration of 6 wt%(Table 1). A similar trend in terms of textural properties was obtained in aerogels from alginate and alginate composites, like alginate-pectin microspheres generated with different alginate-to-pectin proportions[36]. Table 1 Textural properties of aerogel-based scaffolds from inks at different alginate(6,8, 10 wt%) concentrations and crosslinked in gelation baths of different CaCl2(0.1, 0.5, 1 M) concentrations. Notation: ABET: specifci BET surface area, dp:BJH-mean pore diameter, Vp: BJH-specifci pore volume. Aerogel scaffold ABET(m2/g) dp(nm) Vp(cm3/g) Alg 6%, HA 0%, CaCl2 0.1 M 438 ± 22 22 ± 1 3.14 ± 0.16 Alg 6%, HA 0%, CaCl2 0.5 M 277 ± 14 22 ± 1 2.00 ± 0.10 Alg 6%, HA 0%, CaCl2 1 M 183 ± 9 19 ± 1 1.16 ± 0.06 Alg 8%, HA 0%, CaCl2 0.1 M 180 ± 9 17 ± 1 0.95 ± 0.05 Alg 8%, HA 0%, CaCl2 0.5 M 177 ± 9 22 ± 1 1.00 ± 0.05 Alg 8%, HA 0%, CaCl2 1 M 147 ± 7 21 ± 1 0.97 ± 0.05 Alg 10%, HA 0%, CaCl2 0.1 M 172 ± 9 18 ± 1 1.04 ± 0.05 Alg 10%, HA 0%, CaCl2 0.5 M 158 ± 8 16 ± 1 0.87 ± 0.04 Alg 10%, HA 0%, CaCl2 1 M 219 ± 11 14 ± 1 1.11 ± 0.06 3.2. Effect of hydroxyapatite concentration on scaffold morphology Alginate hydrogel printing resulted in stable single fliaments(Fig. 1), but without signifciant binding between layers. Moreover, alginate aerogel scaffolds started to dissolve just after their immersion in aqueous solutions losing their integrity after 24 h. The addition of HA to the alginate ink was hypothesized to preserve the strands geometry while improving structure stability and bioactivity of scaffolds yielding an improved 3D-structure for bone tissue engineering. HA is hydrophobic and the scaffolds would dissolve more gradually under physiological conditions and maintain their shape, at the expense of a reduction in the porosity of the structure[37,38]. To compensate this, alginate aerogels were herein crosslinked at high concentrations of the divalent cations solution(CaCl2 1 M), so that more cations were captured inside the scaffolds and bridged the gel network. Finally, HA is involved in protein adsorption and this process causes cells transportation into the scaffold, which is positive because it may promote cell adhesion and proliferation on scaffold surfaces[39]. Homogeneous 3D-structures were obtained for the HA concentration range tested(0–24 wt%) with fbiers and layers consistently arranged. The macroporous and mesoporous structures of the scaffolds were maintained as well. At higher HA concentrations, more HA granules appear forming the fliaments stacked together with the alginate(Fig. 3). The easy handling of the synthesized alginate-HA scaffolds and the SEM images showing binding between strands appear to confrim the struc-tural integrity and stability of the aerogels after 3D-printing. N2 adsorption-desorption analysis of alginate-HA aerogel scaffolds show an important decrease in the specifci surface area and total pore volume, while the pore diameter is almost unaltered with respect to scaffolds fabricated with alginate only(Table 2). The decrease in the total pore volume could be attributed to the interactions between –NH3groups of alginate and –OH groups and Ca2i ions of HA that lead to the fnial deposition of HA over the scaffold creating an irregular surface structure[16]. In general, the HA addition decreased the textural properties in all alginate-HA formulations, due to the low mesoporosity of the HA powder(2 m2/g). Despite that, the textural properties of the HA-containing alginate aerogels may still be enough to favor cell seed-ing and nutrient diffusion throughout the scaffold structure. The results obtained in terms of textural parameters after the addition of HA are coherent with previous studies using other polymeric scaffolds[16,40]. Apparent density values increased gradually with the addition of HA resulting in a reverse effect on porosity, although all aerogel scaffold formulations tested reached values above 80%(Table 2). The porosity of Fig. 2. SEM pictures of 3D-printed alginate aerogels prepared from 6 wt% aqueous alginate inks and at different CaCl2 concentrations: a) 0.1, b) 0.5 and c) 1 M. Aerogels are observed at two different magnifciations. Fig. 3. Images and SEM pictures of 3D-printed alginate-HA aerogels prepared from 6 wt% alginate inks with different HA concentrations:(a) 0,(b, e) 8,(c, f) 16, and (d, g) 24 wt%. In all cases the gelation was performed using 1 M CaCl2 solutions. Aerogesl are observed at two different magnifciations. Table 2 Textural properties of aerogel-based scaffolds processed from 6 wt% alginate inks with different HA concentrations(0, 8, 16, 24 wt%) and crosslinked with CaCl2 1 M solution. Notation: ABET: specifci BET surface area, dp: BJH-mean pore diameter, Vp: BJH-specifci pore volume, Papp: apparent density, Pskel: skeletal density, e: scaffold porosity, ef: aerogel fbiers porosity. Aerogel scaffold ABET (m2/g) dp (nm) Vp (cm3/g) app (g/ mL) skel (g/ cm3) E (%) Eff (%) Alg 6%, HA 0%, CaCl2 1 M 183 ± 9 19 ± 1 1.16 ± 0.06 0.14 ± 0.01 1.18 ± 0.16 88.56 ± 1.29 86.58 ± 2.26 Alg 6%, HA 8%, CaCl2 1 M 118 ± 6 24 ± 1 0.99 ± 0.05 0.24 ± 0.03 1.72 ± 0.09 85.85 ± 1.59 85.25 ± 4.02 Alg 6%, HA 16%, CaCl2 1 M 67 ± 3 26 ± 1 0.60 ± 0.03 0.29 ± 0.04 1.93 ± 0.04 85.06 ± 2.40 79.78 ± 3.92 Alg 6%, HA 24%, CaCl2 1 M 29 ± 2 31 ± 2 0.21 ± 0.01 0.34 ± 0.02 1.72 ± 0.14 80.33 ± 1.19 76.68 ± 3.54 the fbiers also decreased with the addition of HA. The total porosity values of the scaffolds(88.56 to 80.33%) are slightly higher than the aerogel fbiers porosity values(86.58 to 76.68%) as the scaffolds are formed by a 3D-mesh of vertically and horizontally aligned aerogel microfbiers separated by macroporous gaps. These are good results since the addition of HA have strongly affected other textural parameters (ABET) but not porosity. Nevertheless, higher porosity(80–99%) and lower densities(0.02 g/ cm3 as bulk density) values were previously reported for alginate aerogel in the form of microparticles[41–43]. Consistently, the incorporation of HA has advantages(bioactivity, sim-ilarity to human bone mineral phase)[18,19] at the expense of a slight decrease in textural parameters. The volumetric shrinkage of aerogel scaffolds after performing the supercritical drying was tested(Fig. 4) to unveil the infulence of this process in the end aerogel scaffolds. The direct solvent exchange to ethanol resulted in aerogels without high volumetric shrinkage values and with reduced overall processing time. Structures containing HA had a lower volume shrinkage with respect to the formulation without HA (Alg 6%, HA 0%, CaCl2 1 M). These are good results since higher volume shrinkage values(42–65%) have been reported for alginate aerogels obtained by sequential solvent exchanges[44]. 3.3. Dimensional accuracy tests Printing accuracy and SFF indices were employed to assess the reproducibility and the fdielity of the dual processing strategy herein proposed. The values obtained for both parameters are higher when assessed in the alcogels than when assessed in the aerogels(Table 3). This feature was expected since the volume shrinkage reported in Sec-tion 3.2 infulences the dimensional accuracy indices. Nonetheless, the alcogel printing accuracy and SFF values obtained are close to the values previously reported for 3D-printed alginate gels and for other poly-saccharide gels[37,45]. 3.4. Biocompatibility tests for aerogel scaffolds BALB cells were cultured in the presence of alginate-HA aerogel scaffolds for cell cytotoxicity evaluation. Fig. 5 represents the cell viability after culture for 24 and 48 h with values reaching ca. 100% for alginate aerogels, which means that they had no negative effect on cell proliferation. Similar results on BALB cells viability after 48 h were found for alginate-HA aerogels, regardless of the HA concentration. In general, these viability results indicate that neither the scaffold Fig. 4. Volume shrinkage (in percentage) of different alginate-HA formulations. Table 3 Printing fidelity indices of aerogels prepared from alginate-HA formulations. Aerogels were manufactured at an alginate concentration of 6 wt%, at different HA concentrations(0, 8, 16 and 24 wt%) and at a CaCl2 concentration of 1 M. Aerogel Alcogel Printing Aerogel Printing Alcogel SFF Aerogel SFF scaffold Accuracy(%) Accuracy(%) Alg 6%, 77.73 ± 11.03 43.56 ± 12.94 0.82 ± 0.08 0.64 ± 0.05 HA 0%, CaCl₂ 1 M Alg 6%, 75.51 ± 8.54 39.06 ± 10.70 0.81 ± 0.05 0.62 ± 0.04 HA 8%, CaCl₂ 1 M Alg 6%, 83.51 ± 2.29 50.18 ± 6.05 0.86 ± 0.02 0.67 ± 0.03 HA 16%, CaCl₂ 1 M Alg 6%, 83.35 ± 6.21 48.14 ± 4.84 0.86 ± 0.05 0.66 ± 0.02 HA 24%, CaCl₂ 1 M Fig. 5. Cell viability tests of alginate-HA aerogels. Viability(expressed in%) of BALB cells after 24(grey bars) and 48 h(black) of contact with scaffolds determined by the WST-1 test. There was no statistically signifciant differences among groups(t-test; p 0.05). composition nor the dual processing strategy compromised the cell viability. The high cell viability observed after the tests confrimed the non-toxicity of the aerogel structures and correlates with scaffolds containing the same components[46]. Indeed, the biocompatibility of the initial components of the scaffolds(alginate and HA) was already reported[47]. Overall, these are promising results since cytocompati-bility and a suitable microstructure(pore size and porosity) govern the properties of an ideal scaffold. 3.5. Cell attachment and proliferation tests on aerogel scaffolds A challenge in tissue engineering is the generation of biomaterials with an adequate structure to act as a substrate for cell bonding, multiplication, development and reproduction[48]. MSCs attachment and proliferation in aerogels were herein tested as this cell line is attractive for tissue engineering applications aiming at the generation of artifciial bone substitutes. MSCs present self-renewal potential, they can differentiate in vivo and ex vivo into different cell types like chondrocytes or osteoblasts and their isolation is not related to donor-site morbidity [49]. In the case of osteoblasts, their attachment to scaffolds depends on CaCl: 1M CaCl:1M CaCl:1M CaCl:1M Fig. 6. Confocal microscopy images of DAPI-stained MSCs seeded on aerogel scaffolds and cultured for(a) 6, and(b) 13 days.(c) Cell attachment and proliferation tests of alginate-HA aerogels after 6(grey bars) and 13(black) days of culture in MSCs. the surface area and the porosity of the materials. No differences in MSCs attachment and spreading were observed between aerogel formulations in terms of nuclei staining(Fig. 6). The presence of HA in the scaffolds did not infulence MSCs attachment as previously observed for structures with similar composition[46,49]. Nevertheless, for higher HA concentrations (16 and 24 wt%) the attachment decreases at 6 and 13 days probably due to the high su-perfciial roughness and irregularity that generally favor cell attachment (HA concentration of 8 wt%) but at such higher levels it could make it hard for MSCs to proliferate fully attached to the aerogel. A proliferation tendency is observed for all aerogel formulations, since more nuclei were stained after culturing scaffolds for 13 days than after 6 days(Fig. 6). This feature indicates that scaffolds were non-toxic, biocompatible, suitable for the attachment and growth of MSCs and able to promote cell adhesion and proliferation, as well as the cell coloni-zation of the scaffold. Small pore diameters and high surface areas as oobbttaaiinneedd ffoorr tthhee aaeerrooggeellss ooff tthhiiss wwoorrkk aarree ssuuiittaabbllee ffoorr oosstteeoobbllaasstt attachment because these conditions allow cell interpenetration. 3.6. Cell migration test Fig. 7a–f shows the evolution of the wound closure process after the scratch test with BALB cells in the presence of different aerogel formu-lations. Fig. 7g shows the increase in BALB cell migration in the presence of aerogel scaffolds with respect to the positive control. These are good results since the well-known bioinert properties of alginate make it hard to be degraded in vivo and this feature could have restricted cellular adhesion and migration as previously reported[50]. In general, struc-tures that are stable, with satisfactory morphology and pore size allow signifciant human fbiroblast migration in wound closure in vitro assays [51]. Nevertheless, fniding the best microarchitecture for cell migration in tissue regeneration is still challenging. In previous studies, human dermal fbiroblast migration with alginate composites showed a high closure of the scratch[51]. Furthermore, alginate composites combined with Ca2+ cations resulted in an enhancement on fbiroblasts migration like the herein observed, probably due to changes in the regulation of genes involved in the wound healing process carried out by fbiroblasts. Finally, as chemotaxis is an inherent response of cells it was hypothe-sized to be involved in the cell migration process since the higher con-centration of biochemical factors secreted by injured tissues activate the surrounding cells and stimulate the migration of cells[52]. This bio-logical response could also play a signifciant role in the increase of the migration of fbiroblasts in the presence of alginate-based aerogels herein observed. 4. Conclusions Alginate-HA aerogel scaffolds were successfully fabricated with a precise and customized nanostructure by the combination of 3D-print-ing and aerogel technologies. This technological combination resulted Alg 6%, HA 16%,CaClz1M Alg 6%, HA 24%,CaClz1M Fig. 7. Microscopy images of in vitro scratch test on BALB cells treated with different aerogel formulations and cultured for a) 0 h, and b–f) 24 h. g) Quantitative analysis of the stimulation of BALB cells migration by alginate-HA aerogels after 24 h in cell culture. in nanostructured and dual porous alginate aerogels of interest for tissue engineering applications. 3D-structure is conserved after all processing steps and alginate, HA and CaCl2 concentrations determine scaffold texture. An optimized scaffold formulation must provide a long-term stability and the required biocompatibility for tissue engineering ap-plications. Cell viability tests revealed no toxicity effect or negative impact on BALB cells on normal cell environment because of the pres-ence of the scaffold formulations. Furthermore, fbiroblasts also suc-cessfully accomplished the migration process when cultured with the aerogel formulations herein proposed. MSCs were able to attach and proliferate on alginate-HA aerogels upon culture for 6 and 13 days. All these features are highly desirable for scaffolds to act as temporary supports and harbor the bone regeneration process. Finally, the fdielity of the end aerogel scaffolds with respect to the original CAD is high. Consistently, the macroporous alginate-HA aerogel scaffolds obtained by this novel technological combination of 3D-printing and supercritical drying methods represent a promising alternative for bone regenerative applications opening up new possibilities to personalized medicine. Other requirements to accomplish bone tissue formation like the degradation rate of the 3D-structures and their mechanical properties will be optimized in a future work. Supplementary data to this article can be found online at https://doi. org/10.1016/j.msec.2021.112525. Acknowledgments This work was supported by Xunta de Galicia[ED431C 2020/17], MICINN[PID2020-120010RB-I00], Agencia Estatal de Investigacioon [AEI] and FEDER funds. Work carried out in the framework of the COST Action CA18125 “Advanced Engineering and Research of aeroGels for Environment and Life Sciences”(AERoGELS) and funded by the Euro-pean Commission. A.I.-M. acknowledges to Xunta de Galicia for her predoctoral research fellowship[ED481A- 2020/104]. A. Alonso is commended for his technical contribution to this work. Declaration of competing interest References [1] S. Yue, H. He, B. Li, T. Hou, Hydrogel as a biomaterial for bone tissue engineering:a review, Nanomaterials 10(2020) 1511, https://doi.org/10.3390/nano10081511. [2] N. Amiryaghoubi, M. Fathi, N.N. Pesyan, M. Samiei, J. Barar, Y. Omidi, Bioactive polymeric scaffolds for osteogenic repair and bone regenerative medicine, Med. Res. Rev. 40(2020) 1833–1870, https://doi.org/10.1002/med.21672. [3] Z. Wang, W. Kapadia, C. Li, F. Lin, R.F. Pereira, P.L. Granja, B. Sarmento, W. Cui, Tissue-specifci engineering: 3D bioprinting in regenerative medicine, J. Control. Release 329(2021) 237–256, https://doi.org/10.1016/j.jconrel.2020.11.044. [4] V. Santos-Rosales, A. Iglesias-Mejuto, C.A. García-Gonzaalez, Solvent-Free Approaches for the Processing of Scaffolds in Regenerative Medicine 20, 2020. [5] J.C. Boga, S.P. Miguel, D. de Melo-Diogo, A.G. Mendonça, R.O. Louro, I.J. Correia, In vitro characterization of 3D printed scaffolds aimed at bone tissue regeneration, Colloids Surf. B Biointerfaces 165(2018) 207–218, https://doi.org/10.1016/j. colsurfb.2018.02.038. [6] M. Askari, M. Afzali Naniz, M. Kouhi, A. Saberi, A. Zolfagharian, M. Bodaghi, Recent progress in extrusion 3D bioprinting of hydrogel biomaterials for tissue regeneration: a comprehensive review with focus on advanced fabrication techniques, Biomater. Sci. 9(2021) 535–573, https://doi.org/10.1039/D0BM00973C. [7] S. Naghieh, M. Sarker, N.K. Sharma, Z. Barhoumi, X. Chen, Printability of 3D printed hydrogel scaffolds: infulence of hydrogel composition and printing parameters, Appl. Sci. 10(2019) 292, https://doi.org/10.3390/app10010292. [8] A. Dhawan, P.M. Kennedy, E.B. Rizk, I.T. Ozbolat, Three-dimensional bioprinting for bone and cartilage restoration in orthopaedic surgery, J. Am. Acad. Orthop. Surg. 27(2019) e215–e226, https://doi.org/10.5435/JAAOS-D-17-00632. [9] Q. Wang, Q. Xia, Y. Wu, X. Zhang, F. Wen, X. Chen, S. Zhang, B.C. Heng, Y. He, H.-W. Ouyang, 3D-printed atsttrin-incorporated Alginate/Hydroxyapatite scaffold promotes bone defect regeneration with TNF/TNFR signaling involvement, Adv. Healthc. Mater. 4(2015) 1701–1708, https://doi.org/10.1002/adhm.201500211. [10] C.A. García-Gonzlalez, T. Budtova, L. Duraaes, C. Erkey, P. Del Gaudio, P. Gurikov, M. Koebel, F. Liebner, M. Neagu, I. Smirnova, An opinion paper on aerogels for biomedical and environmental applications, Molecules 24(2019) 1815, https:// doi.org/10.3390/molecules24091815. [11] G. Horvat, K. Xhanari, M. Finlsgar, L. Gradilsnik, U. Maver, ZZ. Knez, Z. Novak, Novel ethanol-induced pectin–xanthan aerogel coatings for orthopedic applications, Carbohydr. Polym. 166(2017) 365–376, https://doi.org/10.1016/j. carbpol.2017.03.008. [12] V. Hegeduss, F. Kernenyi, R. Boda, D. Horvtath, I. Laazaar, E. Tooth-Gyoori, B. Dezsoo, C. Hegedus, B-tricalcium phosphate silica aerogel as an alternative bioactive ceramic for the potential use in dentistry, Adv. Appl. Ceram. 117(2018) 476–484, https://doi.org/10.1080/17436753.2018.1498145. [13] M.V. Reyes-Peces, A. Péerez-Moreno, D.M. de-los-Santos, M.del M. Mesa-Díaz, G. Pinaglia-Tobaruela, J.I. Vilches-Peerez, R. Fernaandez-Montesinos, M. Salido, N. de la Rosa-Fox, M. Pienero, Chitosan-GPTMS-silica hybrid mesoporous aerogels for bone tissue engineering, Polymers 12(2020) 2723, https://doi.org/10.3390/polym12112723. [14] V. Santos-Rosales, I. Ardao, C. Alvarez-Lorenzo, N. Ribeiro, A. Oliveira, C. García-Gonzallez, Sterile and dual-porous aerogels scaffolds obtained through a multistep supercritical CO2-based approach, Molecules 24(2019) 871, https://doi.org/10.3390/molecules24050871. [15] T. Budtova, D.A. Aguilera, S. Beluns, L. Berglund, C. Chartier, E. Espinosa, S. Gaidukovs, A. Klimek-Kopyra, A. Kmita, D. Lachowicz, F. Liebner, O. Platnieks, A. Rodríguez, L.K. Tinoco Navarro, F. Zou, S.J. Buwalda 12(2020) 2779, https://doi.org/10.3390/polym12122779. [16] C. Sharma, A.K. Dinda, P.D. Potdar, C.-F. Chou, N.C. Mishra, Fabrication and characterization of novel nano-biocomposite scaffold of chitosan–gelatin–alginate–hydroxyapatite for bone tissue engineering, Mater. Sci. Eng. C 64(2016) 416–427, https://doi.org/10.1016/j.msec.2016.03.060. [17] G. Turco, E. Marsich, F. Bellomo, S. Semeraro, I. Donati, F. Brun, M. Grandolfo, A. Accardo, S. Paoletti, Alginate/Hydroxyapatite biocomposite for bone ingrowth:a trabecular structure with high and isotropic connectivity, Biomacromolecules 10(2009) 1575–1583, https://doi.org/10.1021/bm900154b. [18] Y. Luo, Y. Li, X. Qin, Q. Wa, 3D printing of concentrated alginate/gelatin scaffolds with homogeneous nano apatite coating for bone tissue engineering, Mater. Des.146(2018) 12–19, https://doi.org/10.1016/j.matdes.2018.03.002. [19] S. Wüst, M.E. Godla, R. Müller, S. Hofmann, Tunable hydrogel composite with two-step processing in combination with innovative hardware upgrade for cell-based three-dimensional bioprinting, Acta Biomater. 10(2014) 630–640, https://doi. org/10.1016/j.actbio.2013.10.016. [20] L. Ruixin, X. Cheng, L. Yingjie, L. Hao, S. Caihong, S. Weihua, A. Weining, Y. Yinghai, Q. Xiaoli, X. Yunqiang, Z. Xizheng, L. Hui, Degradation behavior and compatibility of micro, nanoHA/chitosan scaffolds with interconnected spherical macropores, Int. J. Biol. Macromol. 103(2017) 385–394, https://doi.org/10.1016/j.ijbiomac.2017.03.175. [21] J. Barros, M.P. Ferraz, J. Azeredo, M.H. Fernandes, P.S. Gomes, F.J. Monteiro, Alginate-nanohydroxyapatite hydrogel system: optimizing the formulation for enhanced bone regeneration, Mater. Sci. Eng. C 105(2019), 109985, https://doi. org/10.1016/j.msec.2019.109985. [22] M. Domingos, A. Gloria, J. Coelho, P. Bartolo, J. Ciurana, Three-dimensional printed bone scaffolds: the role of nano/micro-hydroxyapatite particles on the adhesion and differentiation of human mesenchymal stem cells, Proc. Inst. Mech. Eng.[H] 231(2017) 555–564, https://doi.org/10.1177/0954411916680236. [23] H. Liu, H. Peng, Y. Wu, C. Zhang, Y. Cai, G. Xu, Q. Li, X. Chen, J. Ji, Y. Zhang, H. W. OuYang, The promotion of bone regeneration by nanofbirous hydroxyapatite/chitosan scaffolds by effects on integrin-BMP/Smad signaling pathway in BMSCs, Biomaterials 34(2013) 4404–4417, https://doi.org/10.1016/j. biomaterials.2013.02.048. [24] X. Tang, H. Zhou, Z. Cai, D. Cheng, P. He, P. Xie, D. Zhang, T. Fan, Generalized 3D printing of graphene-based mixed-dimensional hybrid aerogels, ACS Nano 12(2018) 3502–3511, https://doi.org/10.1021/acsnano.8b00304. [25] Junzong Feng, B.-L. Su, H. Xia, S. Zhao, C. Gao, L. Wang, O. Ogbeide, Jian Feng, T. Hasan, Printed aerogels: chemistry, processing, and applications, Chem. Soc. Rev. 50(2021) 3842–3888, https://doi.org/10.1039/C9CS00757A. [26] H. Maleki, T. Fischer, C. Bohr, J. Auer, S. Mathur, B. Milow, Hierarchically organized biomimetic architectured silk Fibroin–Ceramic-based anisotropic hybrid aerogels for thermal energy management, Biomacromolecules 22(2021)1739–1751, https://doi.org/10.1021/acs.biomac.1c00175. [27] H. Maleki, S. Montes, N. Hayati-Roodbari, F. Putz, N. Huesing, Compressible, thermally insulating, and frie retardant aerogels through self-assembling silk fbiroin biopolymers inside a silica structure—an approach towards 3D printing of aerogels, ACS Appl. Mater. Interfaces 10(2018) 22718–22730, https://doi.org/10.1021/acsami.8b05856. [28] V. Santos-Rosales, G. Alvarez-Rivera, M. Hillgaartner, A. Cifuentes, M. Itskov, C. A. García-Gonzaalez, A. Rege, Stability studies of starch aerogel formulations for biomedical applications, Biomacromolecules 21(2020) 5336–5344, https://doi. org/10.1021/acs.biomac.0c01414. [29] H. Tetik, D. Feng, S.W. Oxandale, G. Yang, K. Zhao, K. Feist, N. Shah, Y. Liao, Z. C. Leseman, D. Lin, Bioinspired manufacturing of aerogels with precisely manipulated surface microstructure through controlled local temperature gradients, ACS Appl. Mater. Interfaces 13(2021) 924–931, https://doi.org/10.1021/acsami.0c19087. [30] .O.E. Akdere, I. Shikhaliyeva, M. Gümüs¸dereliogglu, Boron mediated 2D and 3D cultures of adipose derived mesenchymal stem cells, Cytotechnology 71(2019)611–622, https://doi.org/10.1007/s10616-019-00310-9. [31] C.A. García-Gonzlalez, J. Barros, A. Rey-Rico, P. Redondo, J.L. Goomez-Amoza, A. Concheiro, C. Alvarez-Lorenzo, F.J. Monteiro, Antimicrobial properties and osteogenicity of vancomycin-loaded synthetic scaffolds obtained by supercritical foaming, ACS Appl. Mater. Interfaces 10(2018) 3349–3360, https://doi.org/ 10.1021/acsami.7b17375. [32] Z. Sartawi, K.B. Ryan, C. Waeber, Bone regenerative potential of the selective sphingosine 1-phosphate receptor modulator siponimod: in vitro characterisation using osteoblast and endothelial cells, Eur. J. Pharmacol. 882(2020), 173262, https://doi.org/10.1016/j.ejphar.2020.173262. [33] J. Zhang, X. Liu, H. Li, C. Chen, B. Hu, X. Niu, Q. Li, B. Zhao, Z. Xie, Y. Wang, Exosomes/tricalcium phosphate combination scaffolds can enhance bone regeneration by activating the PI3K/Akt signaling pathway, Stem Cell Res Ther 7 (2016) 136, https://doi.org/10.1186/s13287-016-0391-3. [34] M.P. Batista, V.S.S. Gonçalves, F.B. Gaspar, I.D. Nogueira, A.A. Matias, P. Gurikov, Novel alginate-chitosan aerogel fbires for potential wound healing applications, Int. J. Biol. Macromol. 156(2020) 773–782, https://doi.org/10.1016/j. ijbiomac.2020.04.089. [35] S. Naghieh, M.R. Karamooz-Ravari, M. Sarker, E. Karki, X. Chen, Infulence of crosslinking on the mechanical behavior of 3D printed alginate scaffolds:experimental and numerical approaches, J. Mech. Behav. Biomed. Mater. 80(2018) 111–118, https://doi.org/10.1016/j.jmbbm.2018.01.034. [36] K. Chen, H. Zhang, Alginate/pectin aerogel microspheres for controlled release of proanthocyanidins, Int. J. Biol. Macromol. 136(2019) 936–943, https://doi.org/10.1016/j.ijbiomac.2019.06.138. [37] M.D. Giuseppe, N. Law, B. Webb, R. A. Macrae, L.J. Liew, T.B. Sercombe, R. J. Dilley, B.J. Doyle, Mechanical behaviour of alginate-gelatin hydrogels for 3D bioprinting, J. Mech. Behav. Biomed. Mater. 79(2018) 150–157, https://doi.org/ 10.1016/j.jmbbm.2017.12.018. [38] H.-R. Lin, Y.-J. Yeh, Porous alginate/hydroxyapatite composite scaffolds for bone tissue engineering: preparation, characterization, andin vitro studies, J. Biomed. Mater. Res. 71B(2004) 52–65, https://doi.org/10.1002/jbm.b.30065. [39] J. Sun, H. Tan, Alginate-based biomaterials for regenerative medicine applications, Materials 6(2013) 1285–1309, https://doi.org/10.3390/ma6041285. [40] H.-W. Kim, J.C. Knowles, H.-E. Kim, Hydroxyapatite and gelatin composite foams processed via novel freeze-drying and crosslinking for use as temporary hard tissue scaffolds, J. Biomed. Mater. Res. A 72A(2005) 136–145, https://doi.org/10.1002/jbm.a.30168. [41] M. Alnaief, R.M. Obaidat, M.M. Alsmadi, Preparation of hybrid alginate-chitosan aerogel as potential carriers for pulmonary drug delivery, Polymers 12(2020) 2223, https://doi.org/10.3390/polym12102223. [42] T. Athamneh, A. Amin, E. Benke, R. Ambrus, P. Gurikov, I. Smirnova, C.S. Leopold, Pulmonary drug delivery with aerogels: engineering of alginate and alginate-hyaluronic acid microspheres, Pharm. Dev. Technol. 26(2021) 509–521, https:// doi.org/10.1080/10837450.2021.1888979. [43] R. Subrahmanyam, P. Gurikov, I. Meissner, I. Smirnova, Preparation of biopolymer aerogels using green solvents, J. Vis. Exp. 54116(2016), https://doi.org/10.3791/54116. [44] A. Veronovski, Z. Novak, ZZ. Knez, Synthesis and use of organic biodegradable aerogels as drug carriers, J. Biomater. Sci. Polym. Ed. 23(2012) 873–886, https://doi.org/10.1163/092050611X566126. [45] P. Panraksa, S. Udomsom, P. Rachtanapun, C. Chittasupho, W. Ruksiriwanich, P. Jantrawut, Hydroxypropyl methylcellulose E15: a hydrophilic polymer for fabrication of orodispersible flim using syringe extrusion 3D printer, Polymers 12(2020) 2666, https://doi.org/10.3390/polym12112666. [46] N.A. Kamalaldin, B.H. Yahya, A. Nurazreena, Cell evaluation on Alginate/Hydroxyapatite block for biomedical application, Procedia Chem. 19(2016)297–303, https://doi.org/10.1016/j.proche.2016.03.012. [47] Th.I. Shaheen, A.S. Montaser, S. Li, Effect of cellulose nanocrystals on scaffolds comprising chitosan, alginate and hydroxyapatite for bone tissue engineering, Int. J. Biol. Macromol. 121(2019) 814–821, https://doi.org/10.1016/j. ijbiomac.2018.10.081. [48] K.M. Tohamy, M. Mabrouk, I.E. Soliman, H.H. Beherei, M.A. Aboelnasr, Novel alginate/hydroxyethyl cellulose/hydroxyapatite composite scaffold for bone regeneration: in vitro cell viability and proliferation of human mesenchymal stem cells, Int. J. Biol. Macromol. 112(2018) 448–460, https://doi.org/10.1016/j. ijbiomac.2018.01.181. [49] L. Benning, L. Gutzweiler, K. Troondle, J. Riba, R. Zengerle, P. Koltay, S. Zimmermann, G.B. Stark, G. Finkenzeller, Cytocompatibility testing of hydrogels toward bioprinting of mesenchymal stem cells: cytocompatibility testing of hydrogels, J. Biomed. Mater. Res. A 105(2017) 3231–3241, https://doi.org/ 10.1002/jbm.a.36179. [50] B. Yao, T. Hu, X. Cui, W. Song, X. Fu, S. Huang, Enzymatically degradable alginate/gelatin bioink promotes cellular behavior and degradation in vitro and in vivo, Biofabrication 11(2019), 045020, https://doi.org/10.1088/1758-5090/ab38ef. [51] R. Gallardo-Rivera, M. de los AAngeles Aguilar-Santamaría, P. Silva-Bermúdez, J. García-Loopez, A. Tecante, C. Velasquillo, A. Romaan-Guerrero, C. Peerez-Alonso, H. Vzazquez-Torres, K. Shirai, Polyelectrolyte complex of Aloe vera, chitosan, and alginate produced fbiroblast and lymphocyte viabilities and migration, Carbohydr. Polym. 192(2018) 84–94, https://doi.org/10.1016/j.carbpol.2018.03.044. [52] C. Lin, B. Tao, Y. Deng, Y. He, X. Shen, R. Wang, L. Lu, Z. Peng, Z. Xia, K. Cai, Matrix promote mesenchymal stromal cell migration with improved deformation via nuclear stiffness decrease, Biomaterials 217(2019), 119300, https://doi.org/ 10.1016/j.biomaterials.2019.119300. [53] A. Salerno, C. Domingo, Making microporous nanometre-scale fbirous PLA aerogels with clean and reliable supercritical CO2 based approaches, Microporous Mesoporous Mater. 184(2014) 162–168, https://doi.org/10.1016/j. micromeso.2013.10.019. [54] C.A. García-Gonzaalez, A. Concheiro, C. Alvarez-Lorenzo, Processing of Materials for Regenerative Medicine Using Supercritical Fluid Technology, Bioconjug. Chem.26(2015) 1159–1171, https://doi.org/10.1021/bc5005922. [55] M. Martins, A.A. Barros, S. Quraishi, P. Gurikov, S.P. Raman, I. Smirnova, A.R. C. Duarte, R.L. Reis, Preparation of macroporous alginate-based aerogels for biomedical applications, J. Supercrit. Fluids 106(2015) 152–159, https://doi.org/10.1016/j.supful.2015.05.010.
关闭-
1/9

-
2/9

还剩7页未读,是否继续阅读?
继续免费阅读全文产品配置单
上海迹亚国际商贸有限公司为您提供《用于骨组织工程的 3D 打印海藻酸盐-羟基磷灰石气凝胶支架》,该方案主要用于骨骼中打印海藻酸盐-羟基磷灰石检测,参考标准《暂无》,《用于骨组织工程的 3D 打印海藻酸盐-羟基磷灰石气凝胶支架》用到的仪器有Cellink 生物3D打印机 BIO X、Cellink BIO X6 3D生物打印机。
我要纠错
相关方案




 咨询
咨询